Ever wondered if you know how to identify a meniscus injury? In this article you will learn what meniscuses are, how they are built, the types of damage, the most common symptoms, how the treatment process works and what exercises can help in rehabilitation. We will present different methods of diagnosis and treatment, from conservative to surgical, and suggest how to avoid this painful injury. If you care about the health of your knees and want to know how to take the best care of them, be sure to read the full text.
From this article you will learn:
- The meniscus- structure and function
- Damage to the meniscus - Symptoms
- Damage to the meniscus - Causes
- Diagnostics
- Treatment of Meniscus Injury
- Rehabilitation After Meniscus Injury
The meniscus - structure and functions
There are two meniscuses in each knee - the medial (on the inside) and side (on the outside). These are crescent-shaped structures made of fibrocartilage, which are located between the femur and tibia. They act as natural shock absorbers -. distribute the load, stabilize the joint, as well as protect joint cartilage Against excessive abrasion.
The meniscus has a unique structure - its structure resembles a wedge, with the thicker part on the outside of the joint and the thinner part facing the center. Thanks to the presence of collagen fibers (mainly type I) arranged peripherally and radially, menisci Are resistant to both shear and tensile forces. It is their flexibility and resilience that allow them to perform many functions:
- shock absorption
- load transfer through the knee joint
- joint stabilization
- improving the fit of the joint surfaces
- "lubricating" and nourishing the joint cartilage
In the standing position, the meniscus even carries the 30-55% total load, and their removal can increase the contact area of the bones that make up the joint even o 70%, resulting in an increase in friction between them and leads to degenerative changes.
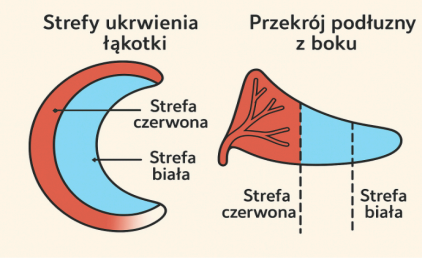
Their content is as much as 74% of water, so that when pressure is applied, they release fluid into the joint cavity, improving slip and reducing friction. In addition, only the outer third (the so-called. "red zone") is well circulated, which is important for treating injuries - it heals better. The inner part ("white zone") is virtually devoid of blood vessels and nourishes itself mainly by diffusion of joint fluid.
Damage to the meniscus - Symptoms
Knee pain during physical activity is often the first signal, indicating possible damage to the meniscus. Although damage to this structure does not always give unambiguous symptoms, there are several typical signs to look out for. Ignoring them can lead to a worsening of the injury and more serious problems with the knee joint.
Most common symptoms of meniscus damage
- Pain on one or both sides of the knee along the joint crevice - It can occur with weight bearing, bending, squatting or even walking.
- "Locking" or "skipping" of the knee - The feeling that the knee does not move smoothly, as if something is blocking its movement.
- Swelling and stiffness - The swelling may occur immediately or build up gradually over several hours.
- A feeling of weakness in the knee - The knee may "run away" or appear unstable.
- Difficulty fully extending or bending the knee - Limited range of motion is one of the more common signals of meniscus damage.
- Audible "click" or "crackle" - may occur at the time of injury and be accompanied by sudden pain.
- Obfuscation - Pain and reduced mobility force a change in gait pattern.
Symptoms may vary depending on From the age of the patient and the type of damage. Younger people are more likely to experience acute sports-related injuries, while older patients struggle with damage from daily activities, leading to micro-trauma and meniscus degeneration.
Damage to the meniscus - Causes
Damage to the meniscus is one of the most common injuries to the knee joint, which can affect both physically active people and those with less active lifestyles. Meniscus injuries can be acute or chronic. Sudden injuries usually occur during intense physical activity, such as twisting the knee with the foot stabilized on the ground - typical in sports such as soccer, basketball and skiing. In addition to the situation described above, damage can occur during:
- sudden twisting or rotation of the knee
- squat with a load
- sudden stop or change of direction
- A direct hit, such as during a slide in
Risk factors:
- Age (especially > 40 years)
- overweight and obesity
- Previous injuries to the knee, especially to the anterior cruciate ligament (ACL)
- contact and dynamic sports
- Work that requires frequent kneeling, crouching or lifting
Types of Damage
Types of meniscus injuries can be divided into several main types, each with its own unique characteristics and challenges in treatment. Although colloquially we simply refer to a "meniscus tear," there are actually many types of ruptures that vary in location, direction and degree of damage.

- Longitudinal damage
- Total cracks - known as "bucket handle tears" (i.e., "bucket handle" type fractures), usually start at the posterior horn of the meniscus and can cover up to 2/3 of its length. They are often unstable and can cause joint locking and mechanical symptoms.
- Incomplete cracks - involving only the upper or lower surface of the meniscus, also usually in the posterior part. They may be asymptomatic.
- Radial (transverse) damage
- The junction of the posterior and medial parts of the medial meniscus
- area of the posterior attachment of the lateral meniscus
- Horizontal damage
This is the most common type of rupture, occurring parallel to the long axis of the meniscus, between the collagen fibers, while perpendicular to the surface of the tibial joint. They are divided into:
Run through Perpendicular to both the long axis of the meniscus and to the articular surface. They cut the collagen fibers which impairs the ability of the meniscus to carry loads.
Typical location:
A progression of this kind is the damage to the so-called "crude". "parrot beak." Such cracks are often not suitable for sewing, and removal of a fragment of the meniscus does not restore its full function. Even a small rupture can lead to more rapid development of degenerative changes.
These cracks run parallel to the plane of the joint, dividing the meniscus into upper and lower parts. They are usually formed as a result of shear forces generated by axial overload. It often develops with age and may be accompanied by the presence of a periarticular cyst. The progression of this type is a lesion of the type "flap"- That is, detachment of the meniscus flap. Meniscus flap can move inside the joint, causing limited range of motion or occasional locking of the joint.
Longitudinal and oblique fractures account for as much as 81% of all meniscus injuries. Most of the changes involve posterior horn of the meniscus, which is most vulnerable to stress. In the case of a knee injury (such as a sprain), it is worth ruling out accompanying damage, such as to the anterior cruciate ligament (ACL).
The type of rupture affects the therapeutic decision - not all ruptures can be sutured, and some require partial removal of a section of the meniscus.
Each of these types of damage requires precise diagnosis using medical imaging techniques, such as MRI, and a personalized treatment plan. The importance of correct diagnosis and the right therapeutic approach is key to successful recovery and minimizing the risk of recurrence.
Diagnostics
The first and most important step in evaluating a patient with knee pain should be a thorough examination interview. Properly asked questions often allow us to determine with great accuracy what kind of injury we are dealing with. In the case of meniscus injuries, the typical mechanism of injury is non-contact injuries, most often resulting from a sudden change in direction, braking or landing after a jump.
With age, the meniscus gradually degenerates, so that even a relatively minor injury can lead to a meniscus rupture - the patient is not always able to pinpoint the specific moment, when did the injury occur. Therefore, it is appropriate to conduct in addition to the interview itself physical examination and if necessary imaging study.
Physical examination
It is one of the most important parts in the diagnostic process of a meniscus injury. In addition to performing specialized provocative tests symptoms of damage to the structure in question, also consists of an assessment:
- swelling, asymmetry, bruising, deformity
- palpation - Soreness in the joint crevice when the knee is bent to 90 degrees on the lateral or medial side is very helpful diagnostically, The sensitivity and specificity of this test are as high as 83%
- range of mobility - Restriction of the range of upright and flexion mobility is a common symptom of the injury depending on the type and extent and symptoms such as swelling
- muscle strength - although strength loss is rarely found with meniscus damage, there may be difficulty performing movements such as single-leg or double-leg squats due to the exaggerated response to compressive forces acting on the knee joint
There are several specialized provocative tests for meniscus injury, here are some of them:
- Thessaly test - The patient stands on one leg, slightly bends the knee (about 20 degrees), and then rotates the trunk and hip left and right. Pain or a feeling of locking of the joint is a possible sign of meniscus damage. Sensitivity: 75%, specificity: 87%.
- McMurray test - In the supine position, the doctor bends the patient's knee as far as possible and then straightens it while rotating the shin. A pop, pain or resistance may indicate an injury. Sensitivity: 61%, specificity: 84%.
- Ege Test - The patient performs a squat, turning the feet outward (if medial meniscus damage is suspected) or inward (if lateral meniscus damage is suspected), tests indicate sensitivity of the test being 64% for injuries to the lateral meniscus and 67% For medial meniscus injuries, with a specificity of 90% and 81%, respectively.





Imaging study
The first step of damage imaging is usually X-rays - w various projections, although they will not show the meniscus injury itself, radiographs are useful in evaluating degenerative changes evaluating degenerative changes and in ruling out other causes of pain, such as fractures or the presence of free bodies in the joint. In the case of arthritic changes, a stress X-ray will also show joint stenosis, osteophytes or subchondral cysts, among others.
In the next stage, the most commonly used imaging study tool is an MRI. The statistics speak for themselves: magnetic resonance imaging shows 93% sensitivity and 88% sensitivity specificity in detecting cracks medial meniscus and 79% sensitivity and as high as 96% specificity in case lateral meniscus. In addition, MRI can determine details such as location, shape, length and depth of the meniscus injury. On images in sagittal sequences sagittal sequences also show differences in the appearance of the lateral and medial meniscus horns - this all of which helps to accurately plan treatment.
The definitive and most precise diagnostic method remains exploratory arthroscopy - That is, direct viewing of the inside of the joint by the surgeon. Due to the invasiveness and risks associated with the procedure, however, it is not performed on every patient. Therefore, MRI, although not without limitations, remains the best non-invasive tool prior to the possible surgery.
Treatment of Damaged Meniscus
Treatment of a damaged meniscus can be carried out in two ways: conservatively or surgically. The choice of the appropriate treatment method depends on:
- types of damage
- degree of damage
- patient's age
- the general condition of the knee joint
- individual patient needs
For smaller injuries, conservative techniques are preferred. Conservative treatment is recommended for meniscus injuries located in well vascularized zones, i.e., the so-called red zone or the peripheral 30% of the meniscus medial meniscus and 25% of the lateral meniscus. The best results are obtained with small ruptures - with a length of less than 5 mm - Which are considered stable and have the greatest potential for potential for spontaneous healing.
Initially, treatment methods include reducing the symptoms that have occurred in the form of: rest, cooling and physiotherapy to minimize stress on the knee joint and reduce inflammation.
On the other hand, in more complicated cases, surgical methods are usually recommended treatment. Over the past 20-30 years, the approach to surgical treatment of meniscus injuries has changed significantly. Increasing emphasis is being placed on meniscus repair and preservation, a not its removal. The goal of modern orthopedics has become to preserve as much of the meniscus, because we know today how important a role it plays in the biomechanics of the knee - it is responsible for cushioning, load transfer, joint stabilization and protection of joint cartilage.
Behavioral Treatment
Conservative treatment of meniscus injury is primarily aimed at avoiding aggravating the injury and ensure the best possible recovery without the need for surgical intervention. surgical intervention. Conservative treatment methods include several key techniques. First, Rest and avoid putting weight on the injured knee are essential to not aggravate inflammation and create the best possible conditions for stimulating the natural regenerative processes. Second, the application of ice several times a day helps reduce swelling and pain in the joint. Another element is physiotherapy, which focuses on strengthening the muscles around the knee and restoring full mobility to the knee joint. Physiotherapists can use a variety of techniques, such as manual therapy, massage functional, medical training or stretching. It is important that conservative treatment is conducted under the guidance of a specialist who will tailor the rehabilitation program to the individual needs of the patient. These treatment methods have key For improving knee joint function and reducing discomfort associated with meniscus damage.
Operative Treatment Methods
Surgical treatments for meniscus injury become necessary for more serious injuries that do not respond to conservative treatment. Thanks to developments in technology and growing awareness of meniscus function, Open meniscectomies made history, and their place was taken by arthroscopic techniques.
Arthroscopy of the meniscus allows precise diagnosis and treatment of the injury with minimal damage to the tissue. This procedure, performed under epidural anesthesia, usually takes 15 to 60 minutes Depending on the complexity of the damage.
There are several possible surgical procedures for meniscus damage:
- Meniscectomy
- Suturing of the meniscus
- Meniscus reconstruction
Total meniscectomy
Although today, total meniscectomy is rarely performed, until a few decades ago it was the standard. The short-term results were good, but as early as 1948 Fairbank pointed out attention to the long-term effects of meniscus removal - the development of degenerative changes and damage to the articular cartilage. We now know that total meniscectomy is associated with an unfavorable prognosis and is considered a last resort.
Partial meniscectomy
When meniscus repair is not possible, it is performed partial meniscectomy, that is, the removal of only the damaged part. Partial meniscectomy remains the most commonly performed procedure, although its long-term efficacy is increasingly questionable. Short-term results (up to 2 years) are usually good - even 80-90% patients experience improvement. However, long-term studies show that it is not an inert procedure -. X-ray degenerative changes appear even in 53% patients after 8 years, compared with compared to 27% in the unoperated knee. The reason for its popularity is the short curve of of learning and quick clinical results, but many surgeons are increasingly turning to techniques repair.
Suturing of the meniscus
In the last three decades The popularity of meniscus repair has increased significantly, and research show that it A more effective and future-proof alternative to meniscectomy. It is now increasingly recommended to try to repair any damaged meniscus that promises to healing - especially in young and physically active people. The most common treatment is arthroscopic suturing of the meniscus, which can be done by three methods:
- Inside-out (from the inside out)
- The advantage is the precision of suturing and the ability to stabilize the posterior horn of the meniscus.
- It requires a small incision at the back of the knee, which increases the risk of nerve and vessels, but allows for a very stable anastomosis.
- Effectiveness: 73-91%.
- Outside-in (from outside to inside)
- Recommended in anterior meniscus injuries.
- Suturing performed by needles inserted through the skin, with the help of an arthroscope.
- The downside can be the difficulty of accurately matching the edges of an extensive crack.
- All-inside (completely from the inside)
- The least invasive option - no skin incisions.
- It uses modern implants (anchors, screws), often biodegradable.
- Faster procedure, fewer complications, but long-term data on effectiveness.
The inside-out and all-inside techniques have gained the most popularity, offering a favorable compromise between the effectiveness and safety of the procedure. Their choice, however, depends on the type and location of the damage.
Meniscus transplant
When all or almost all of the meniscus has previously been removed, and the patient continues to experience pain and limitations - consideration is being given to allogeneic transplant, that is, from a deceased donor or synthetic implant. There are four types of transplant samples: fresh, frozen, freeze-dried and cryopreserved.
The effects of the transplants are evaluated on the basis of:
- pain relief
- improve knee function
- inhibition of degenerative changes
Indications for this type of surgery include primarily patients with complex lesions that do not qualify for suturing. The best results are observed in patients Under 40 years of age, with a straight axis of the limb, a stable knee and minor degenerative changes.
Although transmission of diseases (HIV, hepatitis) is theoretically possible, the procedures used minimize this risk. Also important is the accuracy of the graft size match - the differences are preferred smaller than 5%.
Rehabilitation After Meniscus Injury
Rehabilitation after surgery to remove or repair a meniscus fragment is key element of return to full function after damage to this structure. Both after surgery, as well as conservative treatment, rehabilitation must be individually tailored to the needs of the patient. It requires an advanced approach and close cooperation with an experienced physiotherapist.
The process of meniscus rehabilitation includes a variety of techniques, such as manual therapy, massage but above all the right training. Special attention should be paid to monitoring correct movement patterns, which affect the efficiency of the whole process. It is also important to gradually introduce strengthening and stabilization exercises, to minimize the risk of complications, further injuries and restore full range of motion of the joint knee.
Rehabilitation after meniscus surgery is more than just exercise - it is a thoughtful process that depends on several key factors: type of damage, type of surgery, rate of healing tissues and of course - on the patient's well-being.
But the good news is that after partial meniscectomy (i.e., removal of a portion of the damaged meniscus) can be used fairly intensive and rapid rehabilitation protocol. The procedure itself, however, as previously discussed, is associated with greater follow-up effects in the time perspective.
Unlike repair procedures, in this case there is no need to protect the structure of the meniscus from stress - there is nothing to protect anymore. After partial meniscectomy surgery already in the first week after the operation we begin to gradually load the limb with the help of crutches. Then, for the next 2 weeks, the goal is to regain natural gait and further increasing the mobility of the joint - all in accordance with the patient's perceived ailments. And that means moving forward really fast. First goals as with most orthopedic procedures are to negate the symptoms of the of the procedure such as:
- control of pain and swelling
- maximum recovery of range of motion (ROM) in the knee
- Quick return to full weight bearing on the limb - within the limits of comfort, of course of the patient
An important part of the improvement is the proper strengthening of the key stabilizers of the of the knee joint in particular quadriceps of the thigh. Depending on the level of involvement of the patient's commitment, achieving the appropriate muscle balance predisposing the to return to physical activity such as jumping or running lasts approximately 12 weeks rehabilitation and involves performing a biomechanical functional assessment.
For patients requiring more complex procedures such as suturing or reconstruction, the improvement process also changes. In these types of cases, depending on the depending on the extent of the procedure or the anastomosis used, the main things that change are:
- the possibility of loading the limb
- time to regain full range of mobility
- potential recommendation of orthoses
Regardless of the extent of surgery for patients after arthroscopic meniscus repair the time at which they are most likely to move when belaying crutches partially loading the limb holds Between 4 and 6 weeks of rehabilitation. Also changing is the time in which patients recover full range of mobility of the operated joint- on average 2 weeks longer than after a meniscectomy procedure. When we are dealing with a larger lesion - i.e. a fracture of the length over 3 cm - Rehabilitation requires more caution. In such cases the patient wears a special orthosis that locks the knee joint, which protects against excessive traffic. Only partial loading of the limb, and the range of motion of flexion in the knee is limited for up to 6 weeks.
Return to sports training is possible when the strength of the quadriceps muscle of the thigh in the operated leg reaches at least 80% The strength of the healthy leg regardless of the applied treatment. In contrast participation in sports competitions is recommended only when the strength of this muscle in the operated leg is at least 90% Compared to a healthy leg.
Rehabilitation Exercises
Rehabilitation exercises play a key role in the recovery process after a meniscus injury. The rehabilitation program should include different types of exercises: strengthening, stabilization and stretching. Each type of exercise should be carefully adapted to the stage of rehabilitation and the patient's capabilities.
- Strengthening exercises: aim to rebuild muscle strength around the joint knee. Examples include squats, lunges, and side-to-side leg raises.
- Stabilization exercises: these exercises help improve control of the joint knee, which is especially important during dynamic movements. This can include single-leg exercises and the use of a gymnastics ball.
- Stretching exercises: help maintain and increase range of motion in the joint Knee. Under this term are not only exercises that improve the flexibility of the muscles but also range of motion exercises.
All these exercises should be introduced gradually to avoid overload and allow the tissues to recover at an appropriate rate.
Bibliography:
- Markes AR, Hodax JD, Ma CB. Meniscus Form and Function. Clin Sports Med. 2020 Jan;39(1):1-12.
- Mordecai SC, Al-Hadithy N, Ware HE, Gupte CM. Treatment of meniscal tears: An evidence-based approach. World J Orthop. 2014 Jul 18;5(3):233-41.
- Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, Verdonk R, Darabos N, Ntagiopoulos P, Dejour D, Seil R, Becker R. Management of traumatic meniscus tears: the 2019 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2020 Apr;28(4):1177-1194.
- Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011 Oct;32(30):7411-31.
- Frizziero A, Ferrari R, Giannotti E, Ferroni C, Poli P, Masiero S. The meniscus tear. State of the art of rehabilitation protocols related to surgical procedures. Muscles Ligaments Tendons J. 2013 Jan 21;2(4):295-301.
- Drosos GI, Pozo JL. The causes and mechanisms of meniscal injuries in the sporting and non-sporting environment in an unselected population. Knee. 2004 Apr;11(2):143-9.
- Maffulli, N., Longo, U. G., Campi, S., & Denaro, V. (2010). Meniscal tears. Open Access Journal of Sports Medicine, 1, 45-54.
- Raj MA, Bubnis MA. Knee Meniscal Tears. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
- Bhan K. Meniscal Tears: Current Understanding, Diagnosis, and Management. Cureus. 2020 Jun 13;12(6):e8590.
- Sherman SL, DiPaolo ZJ, Ray TE, Sachs BM, Oladeji LO. Meniscus Injuries: A Review of Rehabilitation and Return to Play. Clin Sports Med. 2020 Jan;39(1):165-183.






