Do you know what the first symptoms of a stroke are? This article will help you understand how to quickly recognize the symptoms and what measures to take to minimize the risk of permanent damage. You will also learn about the most common causes of strokes and how to effectively carry out rehabilitation. All of this is key to protecting yourself and your loved ones from the consequences of this serious disease. Read on to gain knowledge that can save lives.
From this article you will learn:
- Brain Stroke - Symptoms and Causes
- Rehabilitation After Brain Stroke - Key Stages
- Psychological Aspects of Rehabilitation After Brain Stroke

Brain Stroke - Symptoms and Causes
Stroke is one of the most serious medical conditions that requires immediate intervention. It occurs when a blood vessel supplying oxygen and nutrients to the brain becomes blocked by a clot or ruptures. The brain needs a constant supply of oxygen and nutrients, which are delivered with the blood. When blood flow to the brain is interrupted or restricted for some reason, a stroke occurs. Without an adequate blood supply, brain cells begin to die very quickly - and the brain is not the only one that dies. even 1.9 million neurons can die every minute.
Most common symptoms it:
- Paralysis and paresis of the limbs of one half of the body
- speech disorders
- visual disturbances
- cognitive dysfunction
Post-stroke individuals may also experience balance disorders and depressive states. It is worth noting that quick recognition i reaction may significantly impact at course of rehabilitation i reduce risk permanent disabilities. Causes strokes brain are varied, the most common being risk factors such as:
- hypertension
- obesity
- diabetes
- high cholesterol
- cardiovascular diseases
Also lifestyle, including Smoking, stress and lack of physical activity, can contribute to an increased risk of stroke. Even to 80% strokes can prevent, using the appropriate prevention and healthy lifestyle. Therefore, understanding these factors and controlling them are key in stroke prevention.
Symptoms of Brain Strokes
Symptoms stroke are diverse and can involve many systems of the body's functioning. The main symptoms are:
- sudden muscle weakness, paralysis or paresis of one side of the body
- Speech problems such as gibberish speech or difficulty understanding and receiving speech
- memory disorders
- visual disturbances, often in one eye
- balance and coordination problems
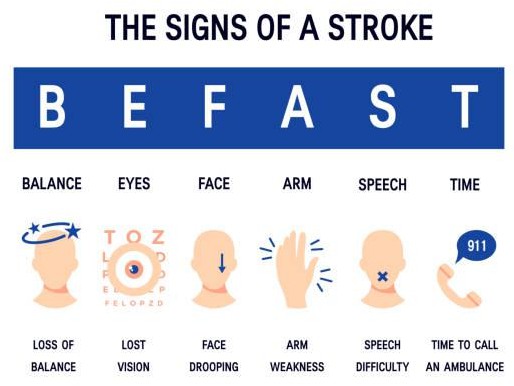
Patients may also experience emergency, strong pain heads, which can be a warning sign for hemorrhagic stroke. Equally important are psychological symptoms, such as abrupt change of mood, confusion or difficulties z concentration. Knowing the symptoms of a stroke is crucial because it allows you to react quickly and call for medical help.
Causes of Brain Strokes
Stroke is the consequence of various factors that can lead to disruptions in the blood supply to the brain. The main types of strokes are ischemic stroke i hemorrhagic stroke.

Stroke ischemic, which represents approximately 80% cases, is caused by a reduction or blockage of the patency of the cerebral artery as a result of a clot encountered, which prevents the delivery of oxygen and nutrients to brain tissue. One of the main causes of ischemic stroke is atherosclerosis, i.e. accumulation of cholesterol deposits (blanks atherosclerosis) On the walls of the arteries. When the plaques become too large, a clot can form, blocking blood flow.
Some people may experience only a temporary disruption of blood flow to the brain, known as a transient ischemic attack (TIA).. A transient ischemic attack (TIA) is a periodic onset of symptoms similar to a stroke, but a TIA does not cause permanent damage. It is the result of a temporary reduction in the blood supply to parts of the brain, which can last only a few minutes. A transient ischemic attack is sometimes referred to as a mini stroke.
In turn hemorrhagic stroke results from leakage or rupture of a blood vessel and hemorrhage into the brain, which occurs in 20% cases.. The spilled blood acts as a bruise - compresses and damages brain cells in a particular area. Risk factors include: hypertension, obesity, diabetes, high level cholesterol, diseases hearts, a also unhealthy lifestyle.
Rehabilitation After Brain Stroke - Key Stages
Post-stroke rehabilitation is a key process that can significantly affect a patient's return to full function. The process is divided into several stages and includes different phases, each with its own specific goals and therapeutic methods.
Neurological rehabilitation may help In improving movement, speech, strength and daily living skills. The post-stroke rehabilitation program aims to restoring independence and improving quality lives. There are many approaches to helping people recover from a stroke. However, there is no one-size-fits-all recipe for post-stroke rehabilitation. Each improvement program is tailored to individual needs and capabilities patient. In general, rehabilitation is based on precisely targeted and repetitive exercises that involve practicing the same skills repeatedly. The sooner you begin post-stroke rehabilitation, the greater the chance of regaining lost skills and abilities.
Usually rehabilitation begins as early as 24-48 hours post-stroke, while in the hospital. The duration of rehabilitation depends on the severity of the stroke and related complications. Some stroke patients recover relatively quickly, but most patients need long-term rehabilitation, which can take several months or years. Rehabilitation methods may depend on:
- the cause, location and severity of the stroke
- The type and degree of post-stroke disorders and disabilities present
- the patient's general state of health
- family and community support
Early rehabilitation, starting as early as the first day of hospitalization, is aimed at preventing complications such as bedsores or contractures and supporting the return of as much function as possible, not only physical but also cognitive, as soon as possible. Rehabilitation after stroke It is divided into three main stages:
- functional prophylaxis (1-21 days after stroke)
- functional rehabilitation (2-24 months)
- Adaptation period (12 months to 5 years)
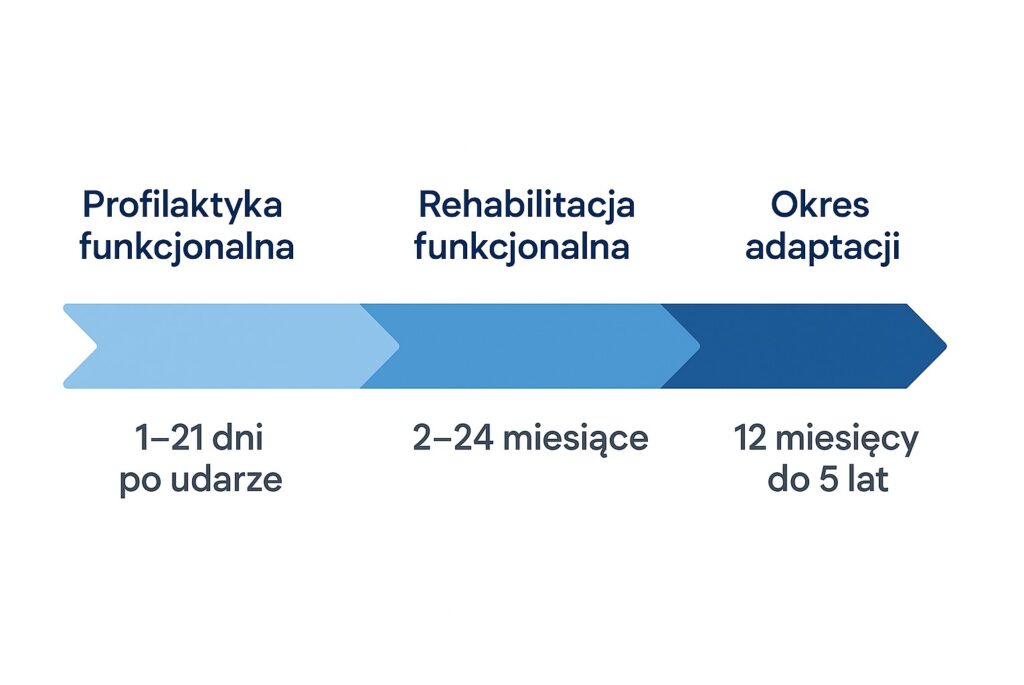
First stage rehabilitation is an important predictor of a patient's ability to regain motor skills in the future. The degree of disability at 2 months after a stroke is usually a reliable indicator of the final outcome. In turn second stage Rehabilitation is the time when the greatest improvement in the patient's functioning occurs, not only physically but also cognitively. In the case of third stage improvement an important goal of rehabilitation is to teach adaptive or compensatory techniques, even if full restoration of motor function is not possible. Training the patient and family in activities such as safe transfers, assisted walking, proper feeding, compensating for speech and language disorders, and providing appropriate adaptive equipment are important goals of rehabilitation.
Rehabilitation at stroke should be carried out systematically and with appropriate continuity and as much intensity as possible from the early stages of improvement in order to maximize support for the recovery process.
First Stage of Rehabilitation
The first stage of post-stroke rehabilitation, lasting from 1 to 21 days, is a critical period in which the main goal of improvement is to get the patient's basic abilities of the body as well as the mind up and running as quickly as possible. During this time, therapists focus on regaining the patient's daily functions by introducing physical exercises Such as: change position in bed, changing the position of the head/ limbs or sitting on the bed.

An important element of improvement in this phase is the appropriate education Both the patient and families/guardians on proper positioning of the patient's body and limb positioning. The goal of patient positioning is to support an optimal rehabilitation process by modulating muscle tone, providing appropriate sensory information and increasing spatial awareness, as well as preventing complications such as limb pain, respiratory problems and supporting safe eating.
One of the simplest forms of stimulation in the acute post-stroke phase is to engage the side paralyzed by the stimuli touch i auditory. It turns out that the right arrangement of furniture and equipment can support rehabilitation. In practice, it gives a better chance to stimulate that side and improve its functioning. A good idea, for example, is to place a cabinet on the paralyzed side. This way, when reaching for objects, the patient has to engage that very side of the body - and this provides stimuli for it. Setting up a chair for the caregiver or visitors works similarly - also on the weaker side.
All this in order to"force" body to be active and stimulate the nervous system to work.
It is worth remembering that auditory stimuli also matter. Conversations, radio and TV sounds should come mainly from the paralyzed side. This supports spatial orientation and stimulates the weaker side of the brain.
Often there is a situation where the family, not knowing how to work and interact with such a person, strengthens thesymptom omissions/ omissions by stimulating the stronger part and communicating with the patient only from this "responsive" side causing the neurons on the paralyzed side to have no opportunity to be stimulated, which can limit their functioning and lead to extensions rehabilitation process, or even worsening prognosis of convalescence.
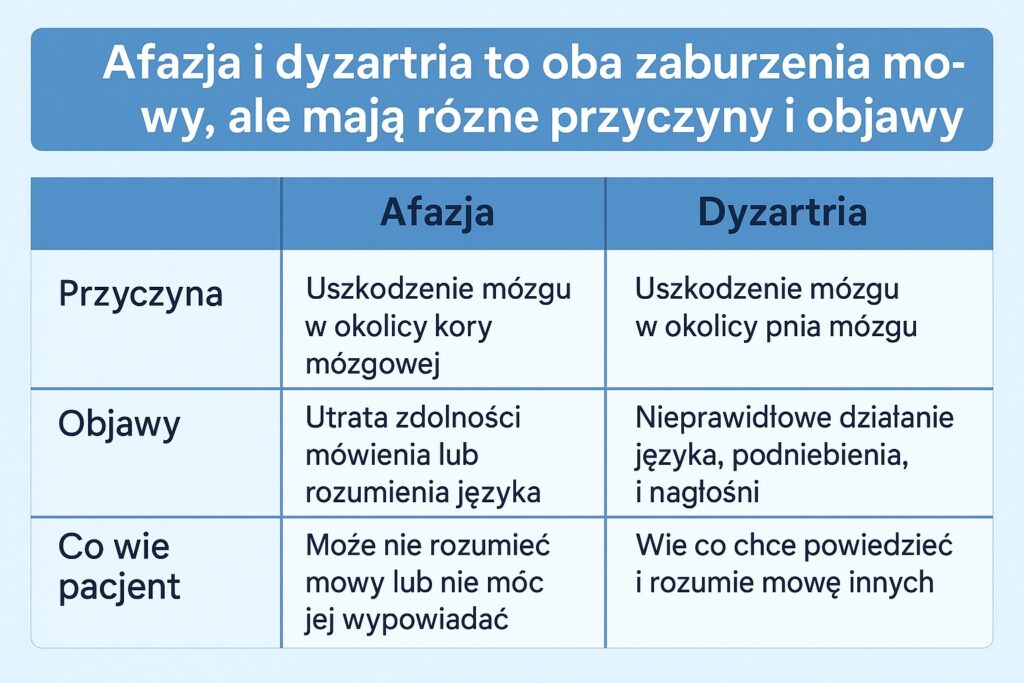
At this stage it is also very important to improve cognitive functions which means practicing communication, writing and breathing. The two main types of speech and language disorders are aphasia and dysarthria. Aphasia is an acquired, multimodal language disorder. It can affect a person's ability to speak, write and understand speech and writing, leaving other cognitive abilities relatively intact. Aphasia is a long-term, life-changing condition that affects both the affected person and others around him or her, in terms of communication style, lifestyle, identity and life roles. It can co-occur with other cognitive deficits. The percentage of stroke cases with aphasia at initial evaluation ranges from 20% to 38%. The speech therapist's role in treating aphasia includes assessment, differentiating aphasia from other communication difficulties, counseling and education to maximize communication, providing alternative or assistive communication, and direct intervention. Dysarthria is a speech disorder of varying severity, affecting speech clarity, voice quality, loudness and overall intelligibility. The incidence of dysarthria after stroke ranges from 20% to 30%, and communication and quality of life can be significantly affected.
Introducing these methods early in the rehabilitation process is crucial for further stages of recovery.
Functional Rehabilitation
The second stage, known as functional rehabilitation, lasts from 1 to as long as 24 months after a stroke. During this period, the goal is to restore lost motor function and improve coordination and muscle strength. Therapists use a variety of exercise techniques, including active, passive and isometric exercises, as well as synergistic exercises to help develop physical fitness.
Functional exercises focus on daily activities such as walking, eating and dressing, allowing patients to gradually return to independence. Regularity and intensity of exercise at this stage are key to achieving optimal therapeutic results. Accordingly, movement tasks are intensified by introducing methods such as:
- general development exercises
- counterbalancing exercises
- gait training
- manual therapy
- occupational therapy (sociotherapy, ergotherapy)
- physical therapy (electrostimulation, whirlpool baths)
- robotics
Using the specific improvement techniques mentioned above, rehabilitation is also beginning to focus on more local problems such as:
- shoulder joint pain
- prevention of shoulder joint relocation
- swelling of the hands
- imbalances
- lower limb spasticity
- management of falls
Bigger or smaller shoulder pain after a stroke occur in 80% patients. Most often these complaints appear in the second phase of improvement after the flaccid stage (>3 week from stroke). Usually this pain is associated with subluxation of the joint, which can lead to inflammation of the subacromial bursa, damage to the tendons of the rotator muscles of the joint, or can be the result of spasticity that occurs at later stages. In such a situation, care should be taken when performing movements involving the painful joint, especially rotational movements, and every effort should be made to protect the shoulder during transfers, positioning the patient and sitting in a wheelchair. Treatment of a painful shoulder resulting from a stroke involves the use of painkillers, nonsteroidal anti-inflammatory drugs, electrostimulation, joint stabilizer activation training, careful and progressive range-of-motion exercises, and sometimes a short treatment with oral steroids. Shoulder pain can prevent the patient from participating in rehabilitation, leading to poorer improvement results. As a result of prolonged pain, it can also lead to depression, insomnia and reduced quality of life.
Spasticity (PSS, Post-Stroke Spasticity). is a common complication after a stroke that causes muscle stiffness and involuntary muscle contractions. It occurs due to damage to the part of the brain responsible for controlling muscle tension resulting in a disruption of communication between the brain and muscles. The area of the brain responsible for controlling muscle tension is the cerebellum and extrapyramidal system.
Depending on the study, its frequency occurrences among post-stroke individuals fluctuates from 19% (Sommerfeld et al., 2004) up to even 92% (Malhotra et al., 2011). During the first year After a stroke, spasticity may occur In approximately 38% patients. According to the data Stroke Association, spasticity affects about one in four post-stroke patients. In the first year after a stroke, there may be a 25-43% patients and is more common in younger individuals.
Classification of spasticity should take into account its scope and distribution in the body. We distinguish:
- focal spasticity
- multifocal
- segmental
- hemispasticity (involving one half of the body)
- Paraspasticity (e.g., both lower extremities)
- generalized spasticity
It is worth noting that spasticity is only one of the possible symptoms of post-stroke movement disorders. It is estimated that it can lead to a significant deterioration in the ability to function independently and quality of life in about 10-12% people with chronic sequelae of stroke.
Spasticity can make daily activities such as washing, dressing and eating difficult. It can also limit balance, coordination and range of motion.When a muscle cannot move to its full extent, surrounding tendons and tissues can shorten and stiffen, leading to further problems.
Symptoms of spasticity
- Feeling of stiffness in arms, fingers, knees
- Difficulty moving hands or arms
- Problems with walking by tensing leg muscles placed in unnatural positions
- Weakening of motor skills
- Excessive reflexes (e.g., stronger-than-normal reactions to touch)
- Painful muscle spasms
- Difficulty in stretching muscles
Robotics vs. stroke
For therapy on robotic devices necessary is insightful analysis patient aimed at determining the suitability and validity of use. Every time the use of robotic equipment must be as individualized as possible to provide the right conditions to improve not only the quality of rehabilitation but also the time needed to reach key milestones that are extremely important from the point of view of the patient and his independence. The robots also enable objective monitoring of progress by generating detailed progress reports, thanks to which the process is subject to constant evaluation, not only by the opinion of the physiotherapist or the patient, but by reliable numbers. Supervision of the improvement process allows the creation of individual therapeutic scenarios, which significantly reduces the recovery time. Some of the state-of-the-art robotic rehabilitation equipment used in the process of improving post-stroke patients are:
- Lokomat Pro - is a unique gait re-education device that allows training on a treadmill with the correct gait pattern and dynamic pressure relief. The use of the locomotor not only enables proper and safe gait training under pressure relief, but also prevents the consolidation of pathological patterns at an early stage of rehabilitation.

- Hocoma Armeo Spring - is an upper limb neurorehabilitation device that uses an exoskeleton in coupling with the patient's body, which, by completely relieving the strain on the exercising limb, enables training to improve muscle strength, range of motion and motor skills using the patient's active movements. Rehabilitation on the Armeo device is self-paced with biofeedback, using an extensive library of games designed to support patient motivation.

- Bimeo Pro - is a device that uses virtual reality in training based on the movements of daily life using support from the limb not affected by the dysfunction. It provides great training for activities of daily living in which the patient will initially rely on support from the healthy limb.

Long-term Rehabilitation
Long-term rehabilitation after stroke includes a period of adaptation, which can last from one year to as long as five years. During this time, the patient continues with exercises and therapies to adjust to the new reality and improve the quality of life. Further therapeutic methods are introduced, such as occupational therapy, which helps re-learn daily activities, and psychotherapy, supporting the patient in coping with the emotional and social effects of the stroke.
Physiotherapy also plays an important role in further improving strength, coordination and mobility. Exercising at home post-stroke have numerous benefits, such as greater time flexibility and patient psychological comfort. Continuing rehabilitation in a home setting allows patients to maintain regularity of exercise, which is key to achieving long-term results. For the quality of rehabilitation to be optimal, it is important to create the right exercise environment. This means providing appropriate equipment, such as mats, balls or resistance bands, as well as a space where the patient can exercise freely.
Support from loved ones is also vital, as they can help the patient with more complicated exercises and monitor progress. In many cases, the following are essential practical training z therapist, during which the caregiver learns safe and effective techniques for supporting the patient. This not only helps ensure safety at home, but also boosts confidence in the caregiver and the patient himself.
Patient's home may need to be adapted By introducing appropriate facilities, such as:
- toilet (tank) chair
- bench for bath or shower
- cane, walker or wheelchair
Falls
Falls are one of the main risks for patients during the improvement phase in the home environment. About 40% people Suffers at least one fall during rehabilitation, a 22% these incidents ends in injury. Particularly vulnerable to falls are people with:
- neglect syndrome of one side of the body
- cognitive disorders
- Difficulties with transferring (e.g., from bed to wheelchair)
- Taking sedative and psychotropic drugs
Falls can occur both at home and in public spaces. Their consequences can be serious - the most common complication is breach necks bones femoral, which usually affects the affected side and may occur even much months or years at stroke. This is partly due to losses masses bone related z immobilization i osteoporosis.
Driving after a stroke - an important goal, but not for everyone
For many patients, especially younger patients, return to running vehicles is one of the key goals after a stroke. The decision to resume driving should be made In consultation with the doctor, patient and family, after a thorough evaluation of the possibilities and safety.
Safe driving requires:
- good attention and concentration
- proper vision
- fast response time
Many people experience impairments in these areas after a stroke, so driving should be strongly discouraged in such cases. This is especially true for patients with:
- visual impairment
- one party neglect syndrome
- epileptic seizures
If the only problem is the paresis of one side of the body, it is possible to adapt the vehicle with the help of:
- special handlebar grips
- accelerator and brake pedal extenders
- other individual technical solutions
It is estimated that from 30% to 61% people who were driving before the stroke, returns to driving after illness. One of the most effective tools for assessing driving ability after a stroke is the test practical at way, conducted by an experienced examiner. It allows you to assess with a high degree of accuracy whether your driving will be safe for you and your surroundings.
Back to work
Over 25% post-stroke individuals under 65 years of age returns to professional work. Several key factors influence the success of a return to work:
- white-collar job
- retained cognitive abilities (e.g., memory, concentration, logical thinking)
- ability to move around independently
Before the decision is made to return to work, it is worth considering professional evaluation capabilities professional, including neuropsychological tests, which will assess mental fitness. A successful return to work can also contribute:
- Appropriate adaptation of the workplace (e.g., elevator accessibility, ergonomic workstation),
- Awareness of the effects of the stroke - both in the employee and the employer,
- Making reasonable environmental and organizational adjustments.
Returning to work after a stroke is an important step in the recovery process. It is worth approaching it gradually - for example, starting with part-time work and gradually increasing the working hours. Such a solution allows a smooth return to daily duties. Working again doesn't have to mean returning to exactly the same position or with the same responsibilities. Even if you are unable to perform your job in the same way as before, there may be other options - it is worth discussing them with your employer. Consider whether your current skills, abilities and energy levels match the work you want to do.
Psychological Aspects of Rehabilitation After Brain Stroke
Post-stroke rehabilitation is not only a physical process, but also a psychological one. Psychological support plays a key role in the recovery process, helping patients cope with difficult emotions such as depression and anxiety. After a stroke, patients often struggle with feelings of helplessness and reduced motivation to exercise, which can significantly affect the effectiveness of rehabilitation. Psychologists support patients and their families by offering stress management strategies and improving overall well-being. Understanding the emotional aspects of rehabilitation and integrating psychological support is therefore integral to providing patients with the best possible therapeutic outcomes.
The Role of the Psychologist in Rehabilitation
A psychologist plays an important role in post-stroke rehabilitation, helping patients cope with a wide range of emotions, from anxiety to depression. Psychological support can include individual therapy, group therapy, and education for patients and their families on how to cope with emotional changes. During therapy, the psychologist focuses on building coping strategies that help patients with daily life after a stroke. In addition, psychologists often work with other members of the rehabilitation team to provide a holistic approach to treating the emotional and physical aspects of recovery. This support is key to ensuring that patients not only regain some of their physical abilities, but also improve their mental well-being.
Patient Motivation
Patient motivation is one of the most important factors affecting the effectiveness of post-stroke rehabilitation. Patients with high levels of motivation are more likely to participate regularly in exercise and better able to cope with the difficulties that the rehabilitation process brings. Therapists have a key role in sustaining and enhancing patients' motivation through a personalized approach and tailoring therapeutic plans to the patient's needs and abilities.
-
- Individualized approach: Therapists use motivational techniques, such as setting small, achievable goals and rewarding progress, to help patients stay engaged.
- Psychological consultation: Psychological support can also include working on building a positive attitude and teaching coping strategies for dealing with frustration and emotional difficulties.
- Social support: Patient motivation can also be enhanced by the involvement of family and loved ones, who support the patient at every stage of rehabilitation.
A consistent and motivating therapeutic approach is crucial to the success of rehabilitation and to improving the quality of life of stroke patients.
Neuroport is a place where we combine modern neurological knowledge with an empathetic approach to the patient. Our team of specialists not only monitors the latest stroke treatment guidelines, but also implements advanced rehabilitation methods that help many patients return to full function faster. We rely on individualized therapy plans and ongoing support from loved ones, because we know that successful rehabilitation requires both professional equipment and human involvement. If you want comprehensive care and proven solutions, Neuroport - rehabilitation center is the correct address.
Authors: Krzysztof Pachutko, Jan Molenda, Katarzyna Socha, Maciej Niedziela
Bibliography:
1. Ovbiagele B, Lyden PD, Saver JL; VISTA Collaborators. Disability status at 1 month is a reliable proxy for final ischemic stroke outcome. Neurology 2010;75(8):688Y692.
2. Duncan PW, Zorowitz R, Bates B, et al. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke 2005;36(9):e100Ye143.
3 Turner-Stokes L, Jackson D. Shoulder pain after stroke: a review of the evidence base to
Inform the development of an integrated care pathway. Clin Rehabil 2002;16(3):276Y298.
4. Perrier MJ, Korner-Bitensky N, Mayo NE.Patient factors associated with return to driving post stroke: findings from a multicenter cohort study. Arch Phys Med Rehabil 2010;91(6):868Y879.5. Management of Adult Stroke Rehabilitation Care: A Clinical Practice Guideline. 2005.
American Stroke Association.
6. Francisco GE, Wissel J, Platz T, et al. Post-Stroke Spasticity. 2021 Jan 15. In: Platz T, editor. Clinical Pathways in Stroke Rehabilitation: Evidence-based Clinical Practice Recommendations. Cham (CH): Springer; 2021.
7 Dworzynski K, Ritchie G, Playford ED. Stroke rehabilitation: long-term rehabilitation after stroke. Clin Med (London). 2015 Oct;15(5):461-4. doi: 10.7861/clinmedicine.15-5-461.
8. Li Xiaohong , He Yanjin , Wang Dawu , Rezaei Mohammad J.Stroke rehabilitation: from diagnosis to therapy Frontiers in Neurology Volume 15 - 2024.
9. Comprehensive Stroke Care Program, Department of Neurology and Department of Physical Medicine & Rehabilitation (SCTIMST), Handbook on Stroke Rehabilitation for Physiotherapists.
10 Stroke Foundation, About Stroke, https://strokefoundation.org.au.
11 American Stroke Association, About Stroke, https://www.stroke.org/en/.






